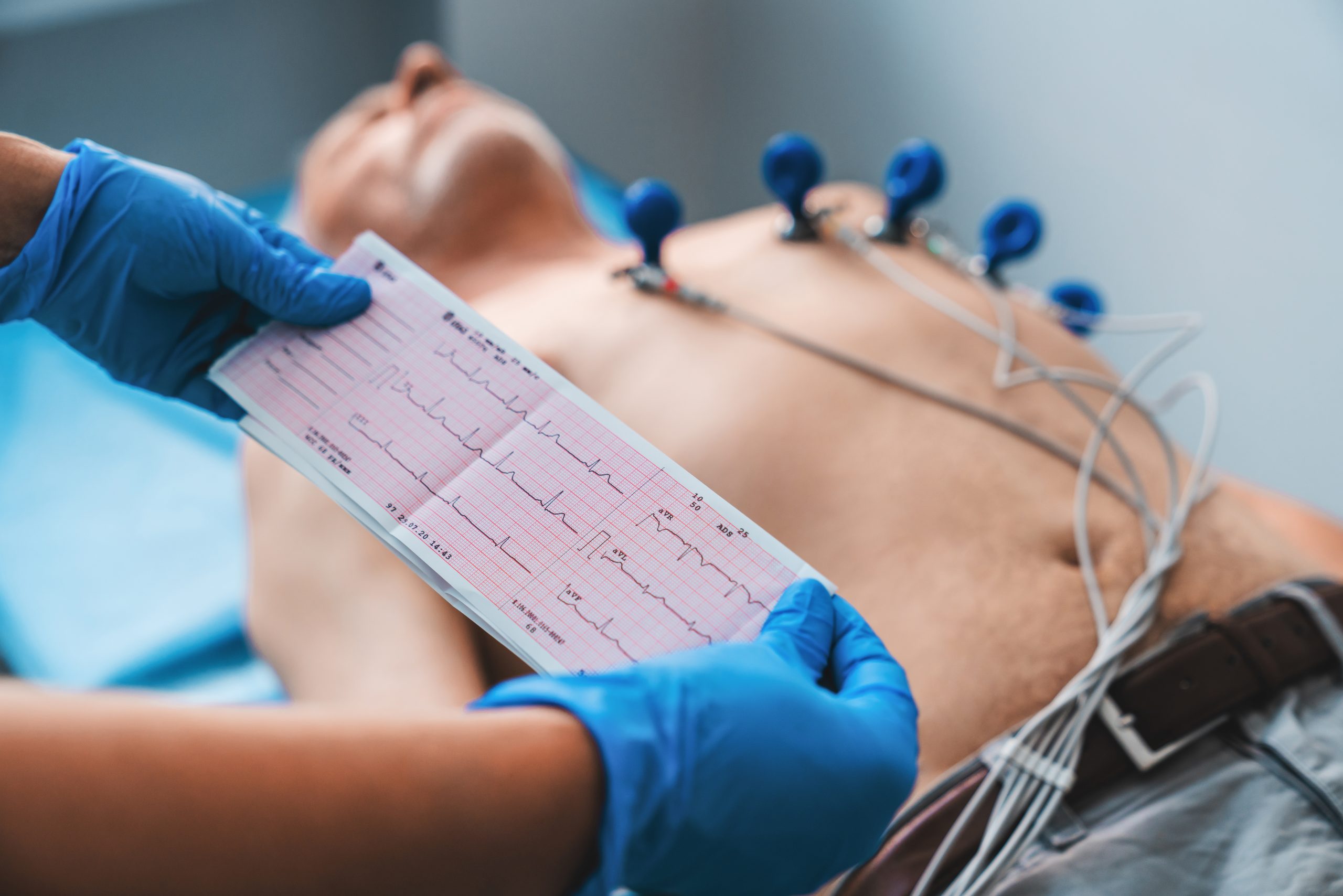
The electrocardiogram (ECG) is a tool that records the electrical activity of the heart, while a stroke is a medical condition that affects the brain due to an interruption in blood flow. Although they may seem unrelated at first glance, there is in fact an important connection between them.
Relationship between electrocardiogram and stroke
Cardiac arrhythmias and stroke
Cardiac arrhythmias are disorders of the heart rhythm that can include irregular, rapid, or slow heartbeats. One of the most common arrhythmias is atrial fibrillation (AF), in which the upper chambers of the heart (the atria) beat rapidly and irregularly.
Mechanism of stroke risk in atrial fibrillation
- Formation of blood clots (thrombi): When the atria do not contract properly due to atrial fibrillation, blood can pool in the heart’s chambers, creating an environment conducive to the formation of blood clots (thrombi). These clots may form in the left atrium, which is the chamber most commonly affected in AF.
- Cerebral embolism: Blood clots formed in the atria can break loose and travel through the bloodstream. If a clot reaches a cerebral artery and blocks the blood flow to a region of the brain, it can cause an ischemic stroke.
- Increased risk of stroke: Atrial fibrillation significantly increases the risk of stroke. It is estimated that people with AF are up to five times more likely to have a stroke than those without this arrhythmia. In addition, strokes associated with atrial fibrillation tend to be more severe and have a higher mortality rate.
Importance of the electrocardiogram in detecting atrial fibrillation
- Early diagnosis: The electrocardiogram is an essential tool for diagnosing atrial fibrillation, as it can detect the characteristic patterns of the arrhythmia, such as the absence of P waves and the presence of irregular fibrillatory waves.
- Continuous monitoring: In some cases, atrial fibrillation can be intermittent and not always evident on a resting electrocardiogram. In these situations, ambulatory cardiac monitoring devices, such as Holter monitors or patch monitors, can be used to detect intermittent episodes of atrial fibrillation and assess the long-term stroke risk.
In summary, the electrocardiogram plays a crucial role in the early detection of atrial fibrillation, a cardiac arrhythmia that significantly increases the risk of stroke due to the formation of blood clots in the heart. Proper identification and management of atrial fibrillation are essential to reducing the risk of stroke and its associated complications.

Heart disease and stroke
Heart disease, which encompasses a wide range of disorders affecting the heart and blood vessels, can significantly increase the risk of stroke. There are several ways in which heart disease can contribute to the development of a stroke:
Atherosclerosis and clot formation
- Atherosclerosis: Heart disease is often associated with the buildup of plaque in the arteries, a process known as atherosclerosis. This plaque buildup can narrow the arteries and restrict blood flow to the brain, increasing the risk of ischemic stroke.
- Clot formation: In addition, atherosclerosis can predispose to the formation of blood clots within the affected arteries. These clots can break loose and travel through the bloodstream to the brain, where they can block a cerebral artery and cause a stroke.
Carotid artery disease
- Carotid stenosis: Heart disease can also affect the carotid arteries, which supply blood to the brain. Carotid stenosis, a narrowing of these arteries due to plaque buildup, can increase the risk of stroke by reducing cerebral blood flow.
Risk of arrhythmias and cardiomyopathies
- Cardiac arrhythmias: People with heart conditions such as heart failure or valvular disease are at increased risk of developing cardiac arrhythmias. These arrhythmias, especially atrial fibrillation, can significantly increase the risk of stroke by predisposing to the formation of blood clots in the heart.
- Cardiomyopathies: Certain forms of heart disease, such as dilated cardiomyopathy or hypertrophic cardiomyopathy, can increase the risk of stroke due to heart dysfunction and the associated formation of blood clots.
Importance of the electrocardiogram and other diagnostic tests
- Assessment of heart disease: The electrocardiogram (ECG), along with other diagnostic tests such as echocardiography and stress tests, can help identify and assess the presence and severity of heart diseases that increase the risk of stroke.
- Comprehensive cardiovascular risk management: It is essential for people with heart disease to receive comprehensive management of cardiovascular risk, which may include controlling blood pressure, cholesterol, and other risk factors, as well as treating cardiac arrhythmias and using anticoagulation when necessary, to reduce the risk of stroke and other cardiovascular complications.
In summary, heart disease can significantly increase the risk of stroke by predisposing to the formation of blood clots, reducing cerebral blood flow, or increasing the likelihood of cardiac arrhythmias. Proper identification and management of heart disease are essential to reduce the risk of stroke and improve overall cardiovascular health.

High blood pressure and stroke
High blood pressure, also known as hypertension, is a major risk factor for both heart disease and stroke. The relationship between high blood pressure and stroke is complex and multifaceted:
Damage to blood vessels
- Arterial stress: High blood pressure exerts excessive force on the walls of the arteries, which can damage them and cause structural changes in their inner lining. This damage can increase the likelihood of atherosclerosis and plaque buildup, which in turn can block blood flow to the brain and cause an ischemic stroke.
- Blood vessel rupture: High blood pressure can also increase the risk of rupture of small blood vessels in the brain, which can lead to bleeding in the brain and a hemorrhagic stroke.
Impact on heart function
- Left ventricular hypertrophy: Chronic high blood pressure can cause thickening of the muscle of the heart’s left ventricle, known as left ventricular hypertrophy. This condition can increase the risk of stroke by raising the likelihood of cardiac arrhythmias, such as atrial fibrillation, and the formation of blood clots in the heart.
Relationship between high blood pressure and atrial fibrillation
- Risk synergy: High blood pressure and atrial fibrillation are independent and common risk factors for stroke. However, when they coexist, the risk of stroke multiplies. High blood pressure can contribute to the development and progression of atrial fibrillation, and atrial fibrillation can exacerbate the effects of high blood pressure on stroke risk.
Importance of detecting and controlling high blood pressure
- Regular blood pressure assessment: It is essential for individuals to undergo regular blood pressure measurements to detect and control high blood pressure. Current treatment guidelines recommend keeping blood pressure below certain thresholds to reduce the risk of stroke and other cardiovascular complications.
- Healthy lifestyle and medical treatment: In addition to medication, controlling blood pressure can also benefit from lifestyle changes such as a healthy diet, regular exercise, weight management, and limiting alcohol and tobacco use.
In summary, high blood pressure is an important risk factor for stroke due to its negative effects on blood vessels, heart function, and its association with other cardiovascular risk factors such as atrial fibrillation. Early diagnosis and proper treatment of high blood pressure are essential to reduce the risk of stroke and improve overall cardiovascular health.
Conclusion
In summary, although the electrocardiogram does not directly diagnose a stroke, it can provide valuable information about heart health and cardiovascular risk factors that may predispose a person to having a stroke. Therefore, it is an important tool in the comprehensive assessment of an individual’s cardiovascular risk and in the prevention of cerebrovascular events.
If you would like more information about NeuroAiD II, please fill out this contact form.
"*" indicates required fields