Cerebral hemorrhages are a medical emergency that require immediate attention due to their potential severity. Understanding what the four types of cerebral hemorrhage are helps clarify their classification, causes, clinical manifestations, and treatments. Each of these types represents a different form of bleeding in the brain, with specific clinical implications that can significantly affect the patient’s prognosis.
What is a cerebral hemorrhage?
A cerebral hemorrhage is the accumulation of blood in the brain or its surrounding areas due to the rupture of a blood vessel. This event can compress brain tissue, disrupt oxygen supply, and impair neurological functions. Common triggering factors include hypertension, traumatic brain injury, vascular malformations, and coagulation disorders.
What are the four types of cerebral hemorrhage?

Answering the question of what the four types of cerebral hemorrhage are involves exploring each of these variants: intracerebral hemorrhage, subarachnoid hemorrhage, subdural hemorrhage, and epidural hemorrhage. Each is described in detail below.
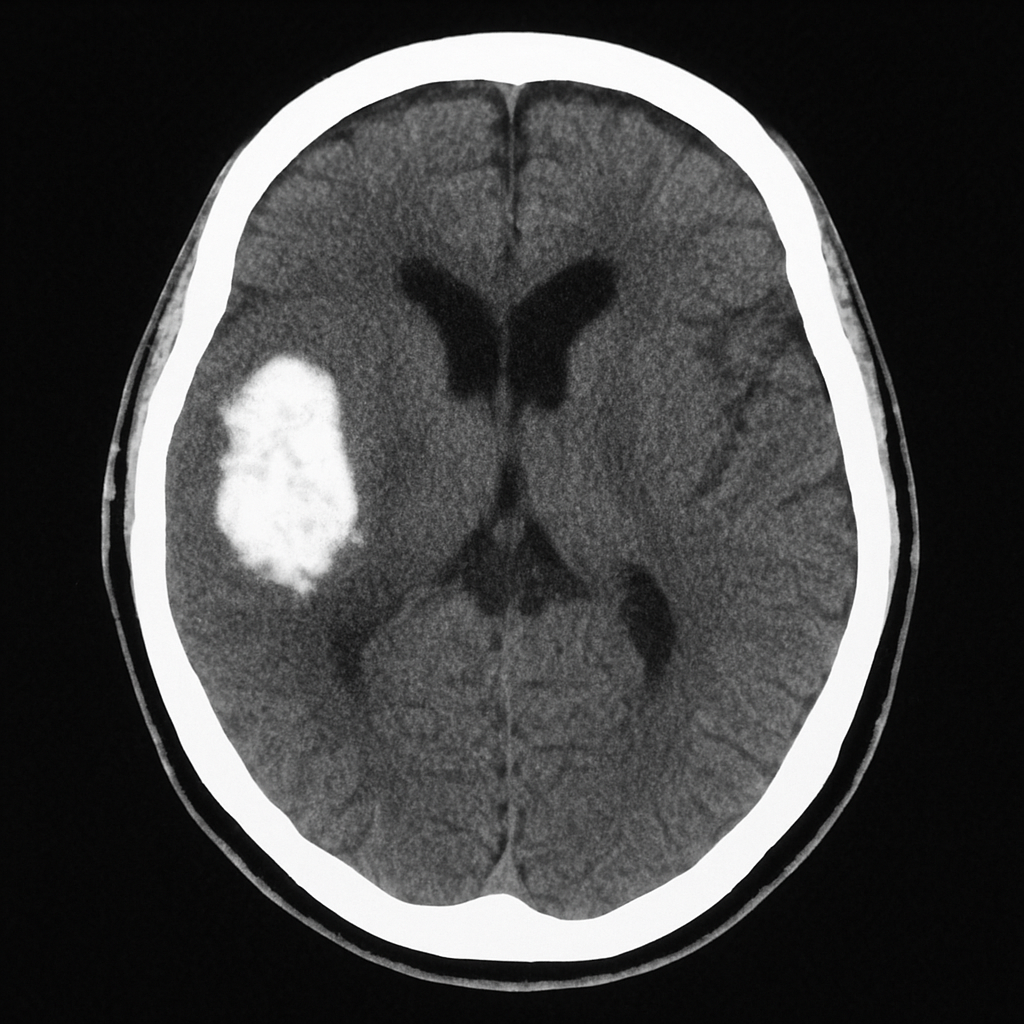
Intracerebral hemorrhage (intraparenchymal)
Intracerebral hemorrhage, also known as intraparenchymal hemorrhage, occurs when a blood vessel ruptures within the brain tissue itself. It is the most common type among spontaneous cerebral hemorrhages.
Main causes:
-
Chronic high blood pressure.
-
Trauma.
-
Arteriovenous malformations.
-
Vascular tumors.
-
Use of anticoagulants.
Symptoms:
-
Sudden neurological deficit (hemiparesis, aphasia, dysarthria).
-
Loss of consciousness.
-
Severe headache.
-
Nausea and vomiting.
-
Seizures.
Diagnosis and treatment:
-
It is diagnosed through computed tomography (CT) or magnetic resonance imaging (MRI).
-
Treatment may be medical (management of intracranial pressure and blood pressure) or surgical in severe cases.
Subarachnoid hemorrhage
This type of hemorrhage occurs when blood accumulates in the subarachnoid space, which is the area between the brain and the arachnoid membrane. It is known for its sudden and dramatic presentation.
Most common causes:
-
Rupture of cerebral aneurysms.
-
Arteriovenous malformations.
-
Trauma.
Characteristic signs:
-
Sudden and intense headache, often described as “the worst headache of my life.”
-
Neck stiffness.
-
Photophobia.
-
Nausea and vomiting.
-
Loss of consciousness.
Diagnosis:
-
Emergency CT scan and lumbar puncture if needed.
-
Cerebral angiography to locate the aneurysm.
Treatment:
-
Surgical clipping or aneurysm embolization.
-
Intensive care unit management with vasospasm control and intracranial pressure monitoring.
Subdural hemorrhage
Subdural hemorrhage occurs when blood accumulates between the dura mater and the arachnoid. It is frequently associated with traumatic brain injuries, especially in elderly individuals or patients with cerebral atrophy.
Etiology:
-
Repeated mild trauma.
-
Falls in the elderly.
-
Prolonged anticoagulation.
Clinical presentation:
-
Slow and progressive onset.
-
Confusion, altered level of consciousness.
-
Hemiparesis or focal symptoms.
-
Personality or behavioral changes.
Forms:
-
Acute: symptoms within the first 72 hours.
-
Subacute: between 3 and 21 days.
-
Chronic: beyond three weeks.
Diagnosis:
-
Cranial CT scan showing a hyperdense crescent-shaped image.
Treatment:
-
In mild cases, observation.
-
In severe cases, surgical drainage through craniotomy or burr hole.
Epidural hemorrhage
Epidural hemorrhage occurs between the dura mater and the skull, usually caused by trauma that ruptures the middle meningeal artery.
Typical cause:
-
Head trauma with temporal bone fracture.
Symptoms:
-
Loss of consciousness followed by a period of lucidity (“lucid interval”).
-
Then rapid neurological deterioration.
-
Dilated pupil on the side of the injury.
-
Contralateral hemiparesis.
Diagnosis:
-
CT scan showing a hyperdense biconvex (lens-shaped) image.
Treatment:
-
Urgent surgical evacuation of the hematoma.
-
Monitoring of vital signs and measures to reduce intracranial pressure.
Differences between types of cerebral hemorrhage
Although all these types are part of the general classification of what the four types of cerebral hemorrhage are, each differs in:
-
Anatomical location of the bleeding.
-
Speed of symptom onset.
-
Causal mechanism.
-
Associated risks and prognosis.
-
Type of medical intervention required.
These differences are crucial for clinical management, as treatment largely depends on the type of cerebral hemorrhage.
Prognosis and rehabilitation
The prognosis of cerebral hemorrhages varies depending on the type, extent of bleeding, speed of diagnosis, and medical care received. Intracerebral and subarachnoid hemorrhages have higher mortality rates. Rehabilitation can be prolonged and may include physical therapy, speech therapy, occupational therapy, and psychological support.
Prevention of cerebral hemorrhages

The best way to prevent these events is to address the risk factors:
-
Control of high blood pressure.
-
Avoiding alcohol and drug abuse.
-
Not smoking.
-
Proper management of diabetes and cholesterol.
-
Prudent use of anticoagulants.
-
Early detection of aneurysms.
Conclusion
Understanding the four types of cerebral hemorrhage—intracerebral, subarachnoid, subdural, and epidural—is essential for quickly recognizing their symptoms, acting promptly, and minimizing neurological damage. Each type presents a distinct challenge in both diagnosis and treatment. Being informed can make the difference between life and death, and between full recovery or permanent aftereffects.
If you would like more information about NeuroAiD II, please fill out this contact form.
"*" indicates required fields