Neuromyelitis optica (NMO), also known as Devic’s disease, is a rare inflammatory disorder that primarily affects the optic nerves and spinal cord. Unlike multiple sclerosis (MS), which also targets myelin in the central nervous system, NMO is distinguished by its clinical course, causes, and underlying mechanisms. The disease can cause episodes of vision loss and muscle weakness, and although it is uncommon, its impact on patients’ quality of life can be significant.
What is neuromyelitis optica (NMO)?
Neuromyelitis optica is an autoimmune disease in which the immune system mistakenly attacks the cells that produce myelin, the substance that covers and protects nerve fibers. The most frequent attacks target the optic nerves and the spinal cord, causing inflammation, vision loss, and muscle weakness.
This disorder often occurs in episodes or relapses, where symptoms may appear and then subside. NMO primarily affects women and is most commonly diagnosed in young adults, although it can also occur in children and older individuals. Unlike multiple sclerosis, relapses in NMO tend to be more severe and often result in more serious long-term effects.
Causes of neuromyelitis optica
The exact cause of neuromyelitis optica is not fully understood, but it is known to be an autoimmune disease. In this type of condition, the body’s immune system mistakenly attacks its own tissues. In NMO, the attack is primarily directed against a protein called aquaporin-4 (AQP4), which is found in the cells responsible for producing cerebrospinal fluid.
The body produces antibodies that attack AQP4, causing inflammation and damage to the affected nerves. These antibodies are present in most patients with NMO, which helps facilitate diagnosis.
Additional factors that may influence the development of NMO include:
- Genetics: Although NMO is not a hereditary disease, some individuals may have a genetic predisposition to developing autoimmune disorders.
- Infections: Certain viruses or infections have been suggested as possible triggers for NMO in genetically predisposed individuals.
- Other autoimmune disorders: NMO may be associated with other autoimmune diseases such as systemic lupus erythematosus or Sjögren’s syndrome.
Symptoms of neuromyelitis optica

The symptoms of NMO vary depending on the part of the nervous system affected and the severity of the autoimmune attack. Relapse episodes are typically marked by:
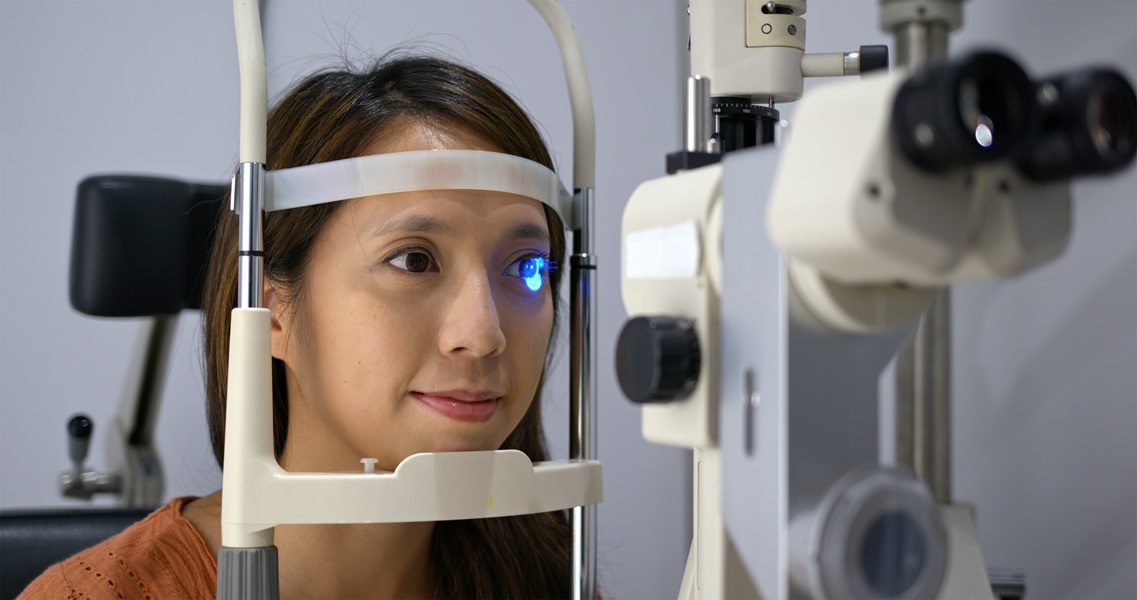
- Vision loss: One of the most common symptoms is optic neuritis, which causes vision loss in one or both eyes. The vision loss may be partial or complete and is often accompanied by eye pain.
- Muscle weakness and paralysis: Inflammation in the spinal cord (transverse myelitis) can cause muscle weakness in the legs or arms, or even paralysis in severe cases.
- Back and neck pain: Transverse myelitis may be accompanied by intense pain in the back or neck due to inflammation in the spinal cord.
- Urinary and digestive problems: Some people with NMO experience difficulty controlling the bladder or bowel due to damage in the spinal cord.
- Severe fatigue: Chronic fatigue is a common symptom in people with NMO and can significantly affect quality of life.
Diagnosis of neuromyelitis optica
Diagnosing neuromyelitis optica can be challenging due to the similarity of its symptoms to other demyelinating diseases, such as multiple sclerosis. Doctors use a combination of clinical and laboratory tests to confirm the diagnosis. The most commonly used tests include:
- Magnetic Resonance Imaging (MRI): MRI allows doctors to visualize inflammation in the optic nerves and spinal cord. Although the lesions in NMO differ from those seen in multiple sclerosis, MRI remains a key tool for diagnosis.
- AQP4 antibody test: This test is crucial for diagnosing NMO, as it detects the presence of anti-AQP4 antibodies in the blood. Approximately 70–80% of patients with NMO have these antibodies, which helps confirm the diagnosis.
- Lumbar puncture: A lumbar puncture may be performed to analyze cerebrospinal fluid for signs of inflammation. Unlike multiple sclerosis, patients with NMO typically have fewer oligoclonal bands, a common marker in other autoimmune diseases of the nervous system.
Treatment of neuromyelitis optica
The treatment of neuromyelitis optica focuses on two main areas: managing acute attacks and preventing future relapses.
- Treatment of acute attacks:
- Intravenous corticosteroids: High-dose corticosteroids, such as methylprednisolone, are used to reduce inflammation during an acute attack. This treatment can provide rapid symptom relief, although it does not always prevent long-term damage.
- Plasmapheresis: If corticosteroids are not effective, plasmapheresis is a procedure that filters harmful antibodies from the blood and can help reduce inflammation.
- Prevention of relapses:
- Immunosuppressants: Medications such as rituximab, mycophenolate, or azathioprine are used to suppress the immune system and reduce the likelihood of future relapses.
- Biologic therapies: Drugs such as eculizumab have shown effectiveness in preventing relapses in patients with NMO. These biologic therapies block the action of harmful antibodies.
Prognosis and quality of life
The prognosis for people with neuromyelitis optica has improved significantly in recent decades thanks to advances in treatment. However, NMO remains a serious disease that can cause permanent disability if not properly managed.

Early treatment is key to preventing long-term damage to the optic nerves and spinal cord. With proper management, many people with NMO can maintain a good quality of life and avoid severe relapses. However, the disease can be unpredictable, and some patients may experience recurrent relapses that require ongoing treatment.
Conclusion
Neuromyelitis optica (NMO) is an autoimmune inflammatory disease that primarily affects the optic nerves and spinal cord, causing vision loss and muscle weakness. Although it is similar to multiple sclerosis, NMO has distinct characteristics and treatments. Advances in diagnosis, such as the detection of anti-AQP4 antibodies, and immunosuppressive therapies have improved the prognosis for people with NMO.
Although it is a chronic disease, proper medical care can help prevent relapses and reduce the impact of symptoms, allowing patients to maintain a more functional quality of life. Ongoing research into biologic therapies and new treatment strategies offers hope for better management of this disease in the future.
If you would like more information about NeuroAiD II, please fill out this contact form.
"*" indicates required fields